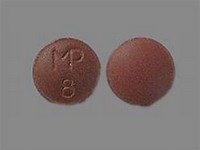
imipramine hydrochloride
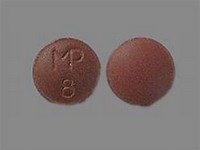
imipramine hydrochloride
CLINICAL USE
Tricyclic antidepressant
DOSE IN NORMAL RENAL FUNCTION
25 mg up to 3 times daily increasing up to 150–200 mg daily; maximum 300 mg in hospital patients
PHARMACOKINETICS
Molecular weight :316.9 %Protein binding :95 %Excreted unchanged in urine : 5 Volume of distribution (L/kg) :31half-life – normal/ESRD (hrs) :9–28/– DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
20 to 50 : Dose as in normal renal function 10 to 20 : Dose as in normal renal function <10 : Dose as in normal renal function DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
CAPD :Not dialysed. Dose as in normal renal function HD :Not dialysed. Dose as in normal renal functionHDF/high flux :Not dialysed. Dose as in normal renal functionCAV/VVHD :Not dialysed. Dose as in normal renal function IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugsAlcohol: increased sedative effect Analgesics: increased risk of CNS toxicity with tramadol; possibly increased risk of side effects with nefopam; possibly increased sedative effects with opioidsAnti-arrhythmics: increased risk of ventricular arrhythmias with amiodarone – avoid concomitant use; increased risk of ventricular arrhythmias with drugs that prolong the QT interval; increased risk of arrhythmias with propafenoneAntibacterials: increased risk of ventricular arrhythmias with moxifloxacin – avoid concomitant use; concentration reduced by rifampicinAnticoagulants: may alter anticoagulant effect of coumarinsAntidepressants: enhanced CNS excitation and hypertension with MAOIs and moclobemide – avoid concomitant use; concentration possibly increased with SSRIsAnti-epileptics: convulsive threshold lowered; concentration reduced by carbamazepine, primidone, barbiturates and possibly phenytoinAntimalarials: avoid concomitant use with artemether/lumefantrineAntipsychotics: increased risk of ventricular arrhythmias especially with pimozide; increased antimuscarinic effects with clozapine and phenothiazines; concentration increased by antipsychoticsAntivirals: increased tricyclic side effects with amprenavir; concentration possibly increased with ritonavirAtomoxetine: increased risk of ventricular arrhythmias and possibly convulsionsBeta-blockers: increased risk of ventricular arrhythmias with sotalol; concentration increased by labetalol and propranololClonidine: tricyclics antagonise hypotensive effect; increased risk of hypertension on clonidine withdrawalDopaminergics: avoid use with entacapone; CNS toxicity reported with selegiline and rasagiline Pentamidine: increased risk of ventricular arrhythmiasSibutramine: increased risk of CNS toxicity – avoid concomitant useSympathomimetics: increased risk of hypertension and arrhythmias with adrenaline and noradrenaline; metabolism possibly inhibited by methylphenidateimipramine hydrochloride.IMIPRAMINe HYDROCHLORIDe 377 ADMINISTRATION
Reconstition
– Route
Oral Rate of Administration
–Comments
– OTHER INFORMATION
Imipramine metabolised to active metabolite desipramine, which has <1% urinary excretion
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home